COVID-19 Local Information
For a word version of the information on this page download (FAQs re Test and Trace for PODs FINALv2 / SOP for PODv2b)
Pharmacy staff testing
A portal for booking COVID-19 tests for key workers, including community pharmacy team members, is now available for use by team members and employers:
Essential workers: apply for a coronavirus test (GOV.UK)
Coronavirus (COVID-19): getting tested – information for employees and employers (GOV.UK)
NHS Test and Trace in relation to healthcare settings
NHS Test and Trace operates a 3-tier system. Where it is known that the case is a healthcare worker (HCW), those cases will be dealt with by Tier 1 which includes Public Health England’s (PHE) local Health Protection Team (HPT). The HPT will receive notification of the case and contact the setting and support the healthcare team to identify and provide advice to the healthcare-related contacts of the positive case (as detailed below). Other contacts of the positive case, for example household or social contacts, will be managed separately via Tiers 2 and 3.
Notification
COVID-19 is a notifiable disease. Healthcare providers should notify PHE of any confirmed cases. NHS primary care providers should also inform their local NHS England and NHS Improvement (NHS EI) commissioning team of any likely interruptions to service delivery. PHE will share information about local cases with the Local Authority Director of Public Health.
Contact details
- Public Health England
Telephone: 0344 2254 524, press the option the Health Protection Team
Email*: ICC.EastMidlands@phe.gov.uk
*All urgent enquiries should be telephoned.
- NHS EI
Pharmacy email: england.eastmidspharmacy@nhs.net
Information that local PHE may ask for when you contact them
1. Details of your pharmacy/practice
-
- name of pharmacy/practice
- address (including postcode)
- key contact details: name, phone number, email
- nature of the pharmacy/practice environment (for example layout, nature of the building, entry/exit, communal areas)
- total number of staff
- number of staff who are clinically vulnerable or extremely clinically vulnerable
- number of staff isolating due to positive test of symptoms
- number of staff admitted to hospital due to COVID-19
- number of staff who have died due to COVID-19
2. Details of the case
-
- contact details of person/s affected
- when the individual(s) became unwell
- when they were last present in the pharmacy/practice
- nature of the roles/job/procedures undertaken by staff affected
- known links between the individual(s) with COVID-19 (in or out of the pharmacy/practice environment)
- number of people with which the individual(s) had close contact
3. Details of control measures
-
- Infection Prevention Control
- PPE
- Social distancing measures
- COVID-19 risk assessments (workplace, staff and patients)
General guide to preventing the spread of COVID-19 in the workplace:
All workplaces are required by law to protect employees and others from harm. A COVID-19 risk assessment must be undertaken in line with the HSE guidance to ensure the safety of the workplace.
Definitions
Case: a confirmed case is laboratory positive case of COVID-19 with or without symptoms
Contact*: a person who has been close to someone who has tested positive for COVID-19 anytime from 2 days before the person was symptomatic up to 10 days from date of onset of symptoms (this is when they are infectious to others). In situations where someone has tested positive for COVID-19 but has not had any symptoms, a contact would be a person who has been close to them anytime from 2 days before the date of test to 10 days after the date of test. For example, a contact would include individuals who:
- Are household contacts
- Have been within a metre of a positive case for a minute or longer
- Have been within 2 metres of a positive case for 15 minutes or longer
- Have travelled in a small car with a positive case
*Please note:
– if the appropriate PPE has been worn properly during an encounter with a case, the staff who came into contact with the case would not need to self-isolate for 14 days. If there is any question about a breach of PPE, then the exposure would need to be risk assessed.
– healthcare workers who have undergone COVID-19 antibody testing and received a positive result must still comply with any instructions to self-isolate as it is not yet known whether a positive antibody test demonstrates immunity.
– face coverings are not considered PPE and therefore if a person (staff or patient) came into contact with a case (staff or patient) whilst wearing face coverings, they would be considered a contact and would need to self-isolate for 14 days.
– there is no guidance supporting immediate mass testing of all staff when informed of a positive case as even if staff test result returns negative, they will still have to self-isolate for 14 days if identified as a contact as the incubation period is from 1 to 14 days.
Outbreak: Two or more confirmed cases linked in time, place and person.
Staff member develops symptoms of COVID-19
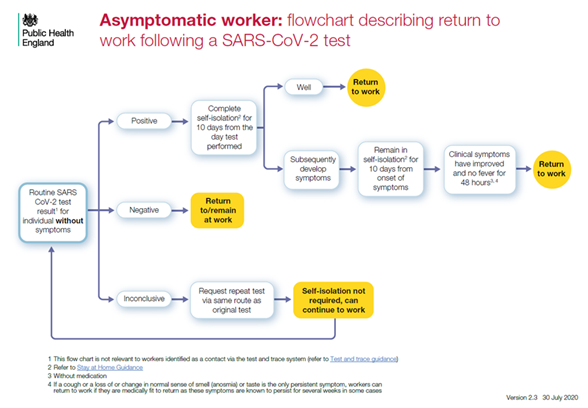
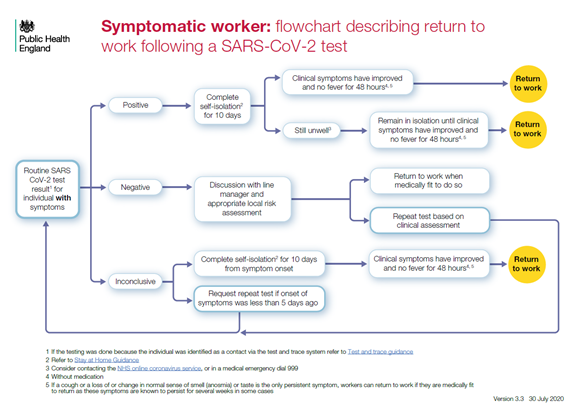
If steps can be taken to mitigate this (eg part time staff increasing their hours temporarily to ensure no interruption to service delivery), there is no requirement to inform NHS EI that staff have developed symptoms of COVID-19. 6. If the affected person tests negative, they can return to work when they are medically fit to do so. For return to work guidance, see Return to work flowcharts: This only applies to individuals who were tested due to having COVID-19 symptoms. It does not apply to individuals who have been tested because they were identified as a contact of a positive case; these individuals still need to complete their 14 days of self-isolation, even if they test negative within that period. Please note that most people who are identified as contacts of a positive case will not be tested, unless they become symptomatic. PHE may however request additional testing in certain situations. 7. If the affected person tests positive, please follow the process detailed in step 2 below for a staff member diagnosed with COVID-19. |
Staff member diagnosed with COVID-19
If an alternative disinfectant is used, ensure it is effective against enveloped viruses. Use disposable cloths or paper roll and disposable mop heads to clean all hard surfaces, floors, chairs, door handles and sanitary fittings. Avoid creating splashes and spray when cleaning. Dispose of all waste from decontamination as Category B waste (not clinical waste) 3. For return to work guidance, see Return to work flowcharts below 4. The pharmacy/practice manager or other appropriate person must notify Public Health England (PHE) of any positive cases they
PLEASE NOTE: The PHE HPTs are extremely busy at present and there may be a delay in them responding to the pharmacy/practice. To avoid any potential further spread of infection whilst awaiting contact from the HPT, the pharmacy/practice should identify contacts of the positive case, consider whether there has been appropriate use of PPE and advise the contacts accordingly of the need to self-isolate (steps below).
These contacts must be advised of the need to self-isolate for 14 days from the point of contact with the positive case and instructed that they do not need to be tested unless they become symptomatic. If they become symptomatic, tests can be requested by calling 119 or online via this website: https://www.gov.uk/guidance/coronavirus-covid-19-getting-tested If a positive test result is returned, isolation period is 10 days from the date of symptom onset, regardless of the number of days in isolation prior to onset of symptoms. If they are symptomatic and their test returns negative, they still need to complete their isolation period. Household contacts of contacts do not need to self-isolate. Once self-isolation period is complete and they have been afebrile for 48 hours, they can return to work: there is no requirement for them to be tested again 5. The pharmacy/practice will be asked to report back to the HPT about the number of contacts identified and whether they have any symptoms. They will also 6. There is no requirement to inform NHS EI of a single positive case if there will be no impact on service provision. If the running of the service is likely to be 7. If the pharmacy/practice becomes aware of 2 (or more) positive cases in staff or members of the public who have attended their healthcare setting, NHS EI 8. Please note that PHE must be informed of all positive cases in a healthcare setting but NHS EI do not need to be informed of a |
Staff member identified as a contact of a positive case outside of the healthcare (workplace) setting
|
To see the most up to date guidance from PSNC and NHSE & I – click here
Check for changes on the flowcharts here – https://www.gov.uk/government/publications/covid-19-management-of-exposed-healthcare-workers-and-patients-in-hospital-settings